Medicare
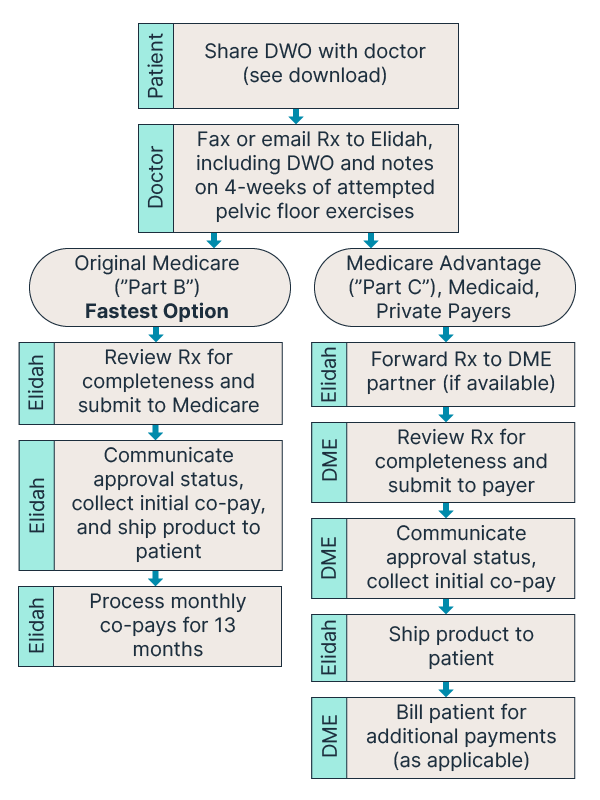
Elitone is approved for nationwide Medicare Part B coverage as Durable Medical Equipment (DME). Medicare covers Elitone as a rental for 13 months, after which ownership transfers to the patient. You will be responsible for any co-pays or out-of-pocket costs.
Requirements for Coverage:
- Prescription for Elitone or Elitone URGE, including a Medical Necessity Statement. See Detailed Written Order (DWO).
- Physician documentation proving a 4-week trial of pelvic floor muscle exercises attempted with additional intervention needed.
- (Preferred) Chart notes supporting the need for neuromuscular electrical stimulation before considering surgical or implantable treatments.
- Prescription Submission: Fax: 833-830-1310 | Email: billing@elidah.com
Note: Medicare Advantage (Part C) follows the same requirements but often requires an in-network, state-specific DME provider. Coverage, co-pays, and availability vary, and we may not have a DME provider for the specific plan.